GP Triage FAQs
How can I request a GP Appointment?
You can go to our website and use our online consultation tool or through the NHS APP. This is the most efficient way to contact the surgery for medical and administrative queries. https://www.thenuffieldpractice.co.uk/
What if I can’t use the internet or need help?
If you are unable to access the online, our team will help fill in the form with you on the phone or you can pop in and speak directly with our reception team who can help you complete the form.
If I ring up/come in, am I more likely to get an GP appointment?
No, all GP appointments will be triaged in the same way, and you will be asked to fill in the form, if you are unable to fill in the form a member of our reception team will be happy to help you.
What about nurse appointments?
These are not changing, and you will still be able to book these by phoning 01993 703641.
Will I see be able to see a GP face to face?
Yes, if the clinical team decide a face-to-face appointment is needed you will be offered one, the online form is a tool to help the clinician triage you request to help ensure you see the correct person or are directed to the appropriate service.
When will I get a response?
For clinical queries submitted using the ‘I have a health problem’, you will receive a response from the surgery the same day. Admin and routine care requests submitted will be reviewed and you will be advised on the outcome within 2 working days.
Is it safe? What happens if my request is urgent?
The AccuRX clinical system is a secure NHS approved system used by GP practices across the country. Medical requests which come in will be triaged by a trained clinician. We are not an emergency service, if you are experiencing a life-threatening emergency, you should call 999.
How will this help me as a patient?
This is a way of managing care requests, designed to ensure that all patients are assessed on clinical need and then directed to the most appropriate care, by the most appropriate person, in the most appropriate timeframe and should help reduce the waiting times, and lead to fewer wasted appointments.
How do I access care when the surgery is closed?
The way you access care when we are close won’t change. Depending on your problem please continue to speak to your pharmacist, use NHS 111, or A&E as before when the surgery is closed or call 999 in an emergency.
Why are we changing our booking system?
Please see this leaflet for information on the reasons for the forthcoming change.
📢 Exciting News: We’re Introducing AccuRx for Online Consultations!
We’re delighted to announce that from 4th December 2025, you’ll have a brand-new way to contact us — through AccuRx, a secure, NHS-approved online consultation platform used by GP practices across the country.
With AccuRx, you’ll be able to contact the practice online for medical or administrative requests using simple, easy-to-complete forms. It’s quick, safe, and designed to make getting help and advice from your GP team even more convenient.
💻 What You’ll Be Able to Do
✅ Submit medical or admin queries online
✅ Receive messages or updates directly from the practice
If you already use the NHS App, you’ll be able to access AccuRx seamlessly through it — making it even easier to stay connected with your care team.
🤝 Need a Hand Getting Started?
Our friendly practice team will be on hand to help!
We know this is a brand-new way to contact us, but don’t worry — AccuRx is simple, secure, and built to work smoothly with the NHS App. We’re here to make sure you feel confident using it from day one
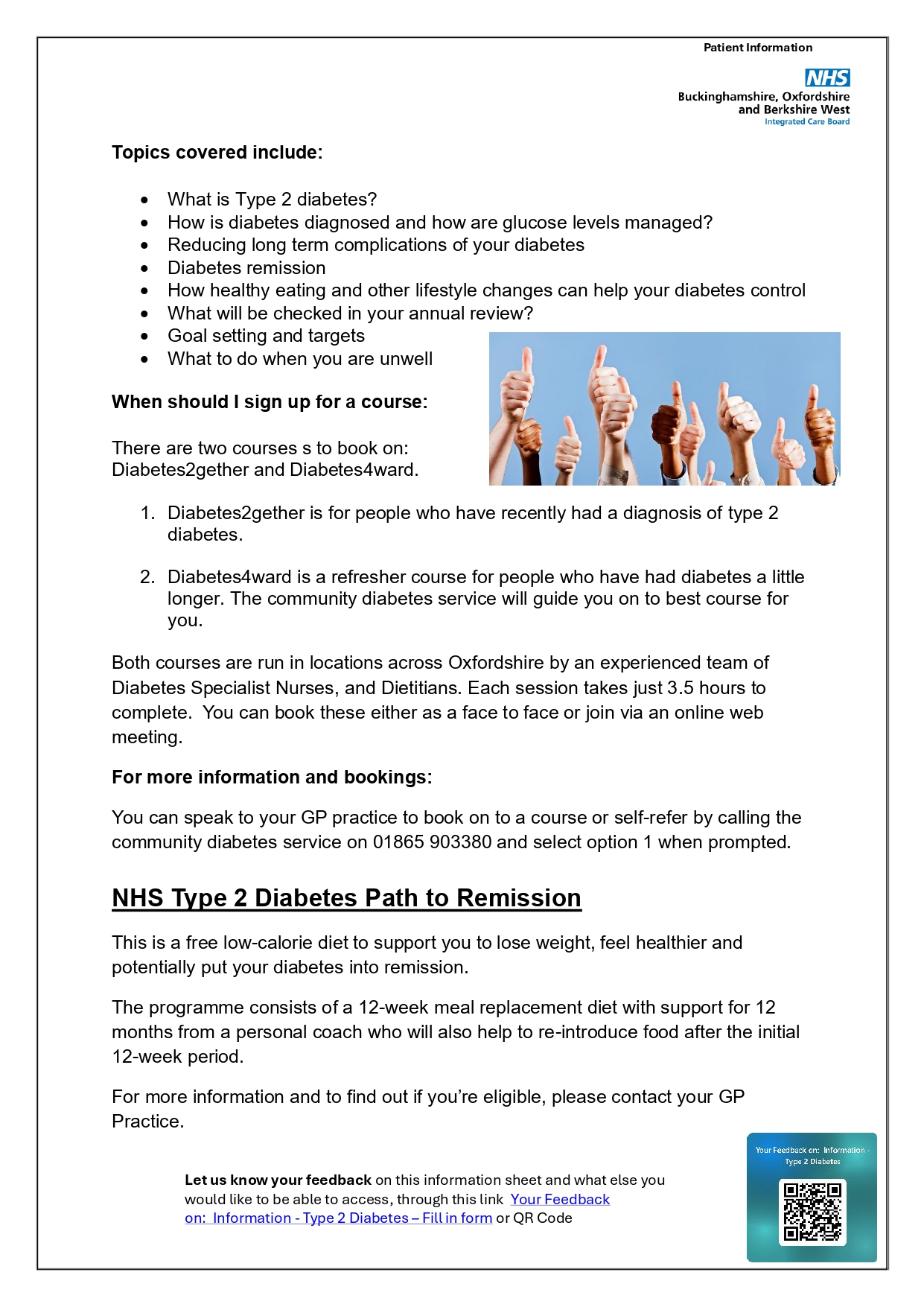
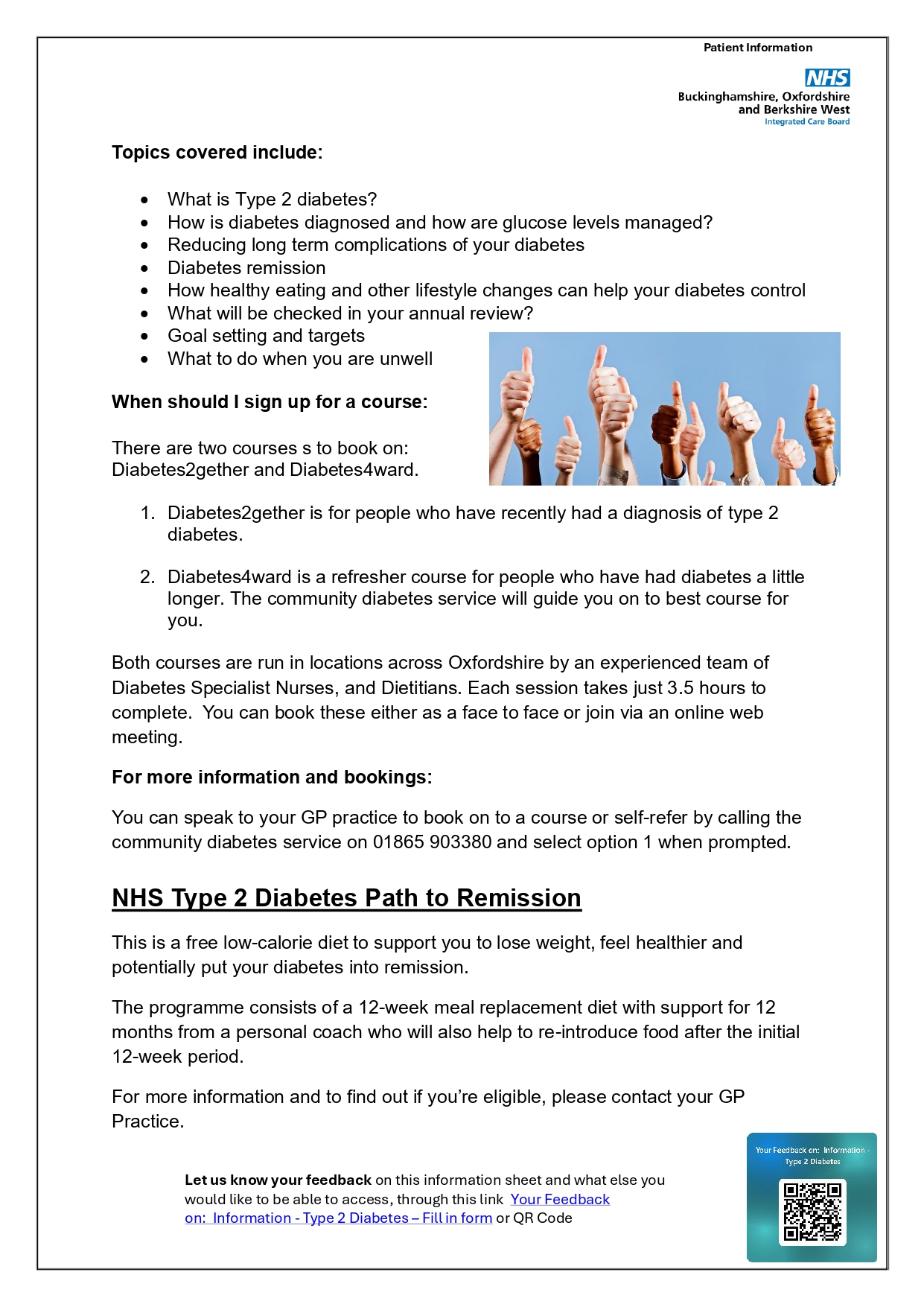
Patient Segmentation
What is segmentation?
We use segmentation to group people based on shared characteristics, needs, or behaviours. This allows us to tailor care delivery and policies to better meet the specific needs of each group.
When we do this for all groups we get healthier people and a healthier population.
What are the John Hopkins Adjusted Clinical Groups?
In BOB we use a well tested set of 11 segments/groups based on research by John Hopkins University. These are in the image above. Factors used for grouping include the number of conditions a person and how severe they are. This helps us decide what level of support they might need.
The categories break down into:
-
Low need (PNG 1-4) - people without significant health issues who need less intervention. Preventative care may stop them becoming unwell.
-
Moderate need (PNG 5-9) - people who have a condition that is well managed. They may need occasional support to remain stable.
-
High need (PNG 10-11) - people who have several conditions. They may need regular monitoring or a more coordinated approach.
You may have seen this score in your NHS App as "John Hopkins adjusted clinical groups system score
As we familiarise ourselves with the new system and adapt to its implementation, we kindly ask that patients refrain from contacting us regarding the reasons behind their assigned ratings. These ratings are automatically generated by an external algorithm and are not within our control.
Weight management: Options available in Witney:
Beezee in Oxforshire: This ‘tier 2’ service is available to adults and children aged 4-12.
- Choose in person sessions, online group sessions or digital
You can refer yourself with this link:
Beezee Adults | Free Healthy Lifestyle Programme
Beezee Familes
Physical activity ‘move together’ referral:
See the following link for more information and to see if you are eligible. You can refer yourself, alternatively we can refer you if you make an appointment with your GP.
Move Together | GO Active
Oviva: This ‘tier 3’ service offering weight loss medications is available for the following people:
- Those who have completed a Tier 2 programme (see above) in the last 2 years
- Those who are medically stable
- BMI >40, or >35 with a weight related condition
You can check your eligibility through the following link:
GLP-1 agonists: treating weight loss with diabetes drugs | Oviva UK
If you think you might be eligible for any of these options or would like to discuss further, please arrange a routine appointment with your GP.
We can also prescribe these weight loss injections (mounjaro) now in the practice (starting July 2025).
Who is eligible?
In the initial phase, NHS England is prioritising access for people with the greatest medical need. This means you must meet all of the following criteria:
- A BMI of 40 or more, and
- At least four diagnosed health conditions linked to obesity from the following list:
- Type 2 diabetes
- High blood pressure (hypertension)
- Cardiovascular disease
- Obstructive sleep apnoea
- High cholesterol or other lipid conditions (dyslipidaemia)
Over time, eligibility may expand, but currently very few people qualify.
What should I do?
- Please don’t contact the GP practice for a prescription at this time – we will contact you if you are eligible.
Thank you for your understanding.
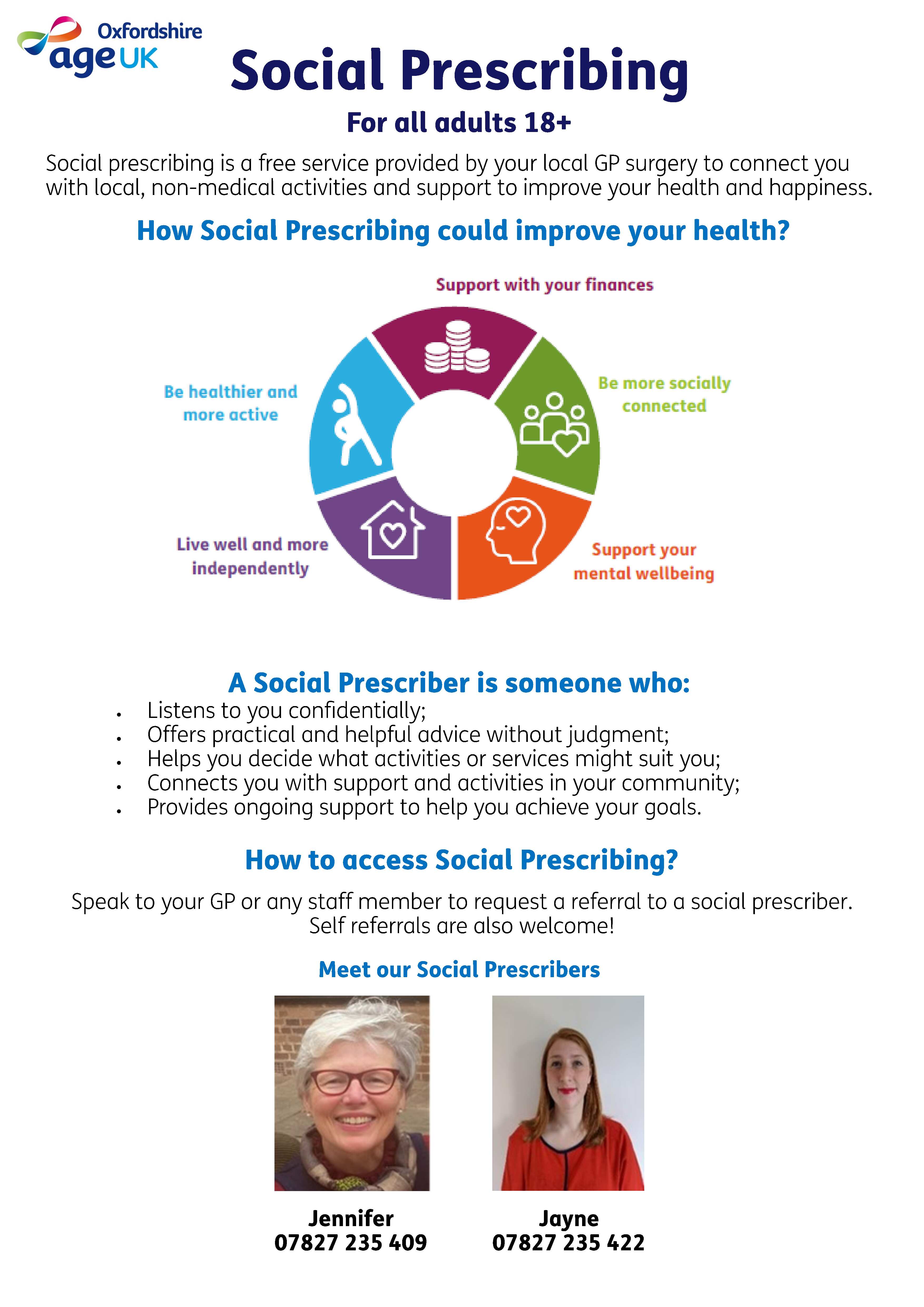
What is social prescribing?
Lots of things can make us feel unwell. Some of these are medical problems that need medical treatment, others are more about the dificulties we all face, at times, in our day-to-day lives.
Social prescribers work with people 18+ and can support you to connect to all the different non-medical services, support, activities and opportunities that exist locally and in your community. They work with you to find support that is tailored to your needs, and which could improve your health and wellbeing, helping you live life to the full.
Oxfordshire Mind is here to support your mental health and overall wellbeing.



Carers Oxfordshire is a free service that offers information, advice and support to unpaid adult carers of someone living in Oxfordshire.
If you are 18 or older and another adult, child or both, relies on you for help to do everyday things, support is available for you.
The support we provide is personalised, enabling you to identify your own needs and make choices about how and when you are supported.
We know that your health and wellbeing are important, so whatever your situation, we want to make caring easier for you.
You can visit the Carers Oxfordshire website HERE
If you have received an invite for your Covid/Flu vaccination, we ask where possible to please use the link to book.
Eligible groups this Autumn
The eligibility is the same across the 4 nations of the UK (England, Scotland, Wales and Northern Ireland).
If you are pregnant or postnatal and would like support to move more in a way that works for you, Move Together is here to help.
Move Together is an Oxfordshire wide programme and is here to support you to move more, to help improve your physical health, mental health and well being.
Please see the posters below for more information.


There have been a small number of cases of MPOX in the UK. Please see the below guidance
Mpox: background information - GOV.UK (www.gov.uk)
Mpox - NHS (www.nhs.uk)
If you have travelled to one of the at risk countries and develop symptoms, please do not attend the surgery but call Reception on 01993 703641, Option 1, who can direct you to a clinician who will assess and triage.
Most eligible adults will be able to get the flu vaccine from 3 October 2024.
This may be later than you've had the vaccine before, but it means you'll have the best protection when flu is most widespread.
Some people may have their vaccination from September 2024, including if:
- you're pregnant (especially if you're near to your due date) – it's important to get vaccinated before giving birth to help protect yourself and your baby for the first few months of their life
- you're due to have treatment that will weaken your immune system (such as chemotherapy) – the vaccine may be given before treatment starts because it works better if given when your immune system is stronger
We will be contacting eligible patients in due course to book their vaccinations.
The Nuffield Practice
Social Media Guidance
There are many social media platforms that are widely used by staff, patients, and members of the public such as Facebook, Twitter, Instagram, YouTube, WhatsApp, and LinkedIn.
Our practice has a Facebook page which provides a range of useful information for our patient population. We have a duty to maintain patient confidentiality and to safeguard vulnerable patients. You can help us achieve this by adhering to the code of conduct outlined in this guidance.
Patients and members of the public are expected to adhere to the following code of conduct at all times:
- Users of portable devices are required to use them in a courteous and considerate manner, that is respectful of others. Unless agreed with the clinician, portable devices should not be used during consultations.
- Information about other patients and staff members is confidential. Patients must not disclose any identifiable information about others on social media without the express permission of that person.
- Patients should not use any social media platform to make or cancel appointments, share medical information with the practice or make contact with a member of staff. Any such contact with the practice should be via appropriately confidential and routine communication methods Contact us - The Nuffield Practice - Witney
- Photographs or any media recordings are not permitted in the waiting room or areas where other patients are present, nor should patients take photographs or media recordings of any staff without their explicit consent.
- Should patients wish to leave a review about The Nuffield Practice , this should be done via the NHS website Find out how to leave a review of an NHS service - NHS (www.nhs.uk) . This will enable the Practice Manager to respond appropriately.
- Patients must not post comments on social media that identify staff who work at the practice.
- Patients must not post any material that is inaccurate, threatening, obscene, defamatory, or unlawful. Any such posts on the practice Facebook page or other social media platforms will be deleted by the Practice and/or reported to the applicable media platform.
Further guidance to this can be found here: https://www.bma.org.uk/advice-and-support/gp-practices/complaints-in-primary-care/dealing-with-abuse-of-practice-staff-on-social-media-from-patients
- Derogatory and offensive comments about our team will not be tolerated on any social media platform. The Malicious Communications Act 1988 and the Communications Act 2003 make it an offence for a patient to send online messages or posts that contain threats, grossly offensive, obscene, menacing, or false information, where the sender’s intention is to cause the recipient distress or anxiety. Legal advice will be sought, and the appropriate action taken against any individual who posts defamatory comments.
Feedback and complaints
We appreciate any feedback our patients may have, good and bad. However, if you wish to make a complaint, we kindly request that you do so using our designated complaints procedure. We will only respond to complaints made to the practice in accordance with the practice policy and a complaint made on any social media platform may be deleted.
Complaints & comments - The Nuffield Practice - Witney
We all know how tough it can be to stay on top of our health, especially during times of stress. It's easy to overdo it and lose track of our drinking habits. But don't worry, DrinkCoach has got you covered.
With DrinkCoach's quick and confidential test, you can easily keep track of your drinking and get personalised advice online. Because at the end of the day, it’s about making responsible choices and taking care of ourselves.
So don't wait any longer, take two minutes out of your day and find out your score today drinkcoach.org.uk/oxfordshire-alcohol-test

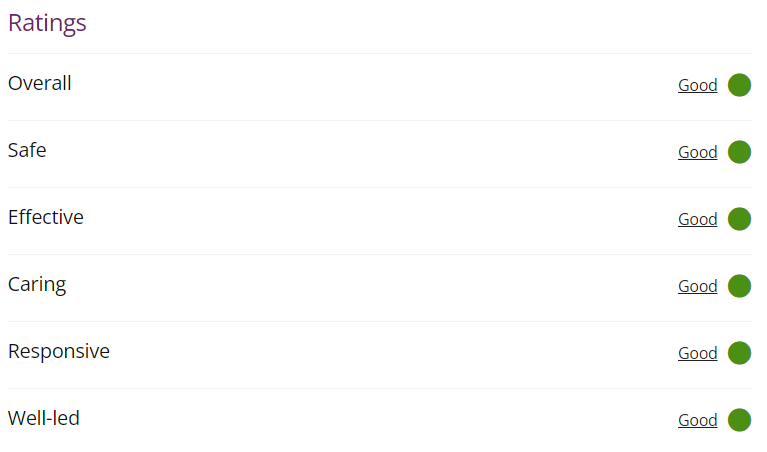
CQC Report - 15th March 2024
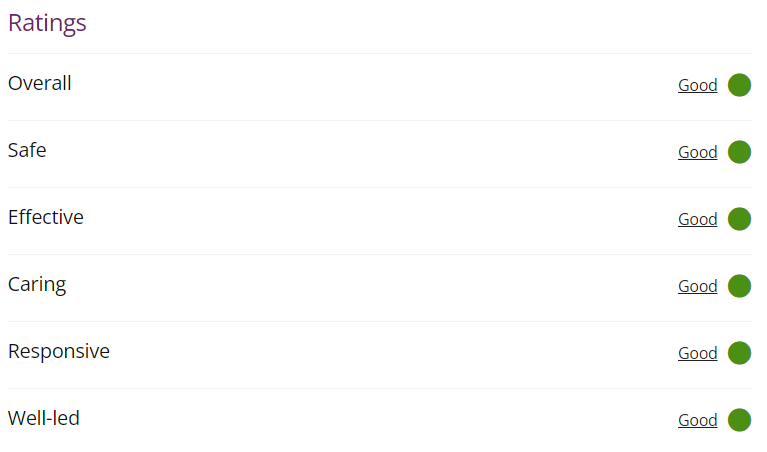
Our view of the service
The Nuffield Practice is a NHS GP practice which provides primary care services to patients in Witney. We carried out an announced assessment of one quality statement, Equity of Access, under the key question of Responsive on 25 March 2024. We carried out the assessment as part of our work to understand how practices are working to try to meet peoples demands for access and to better understand the experiences of people who use services and providers. Overall, the practice is rated as good overall and the key question responsive continues to be rated as providing a good service. We recognise the work that GP practices have been engaged in to continue to provide safe, quality care to the people they serve. We know colleagues are doing this while demand for general practice remains exceptionally high, with more appointments being provided than ever. In this challenging context, access to general practice remains a concern for people. These assessments of the quality statement Equity in Access in the Responsive key question includes looking at what practices are doing innovatively to improve patient access to primary care and sharing this information to drive improvement. Leaders understood the challenges to patient access and used patient feedback and other information to monitor and improve access in a way that met patient needs.
People's experience of this service
Feedback from patients regarding access at the practice was positive as demonstrated from data from the national GP Patient Survey, NHS Friends and Family Test (FFT) and via Give Feedback on Care through the CQC website. A representative from the Patient Participation Group (PPG) reported positive access to services for patients and the practice worked closely with the PPG to continue to identify where they could make improvements.
National guidance expects long-term involvement of specialists in reviewing these patients and their medical treatment, but this does not currently happen in Oxfordshire.
Therefore, in line with county-wide safety recommendations, the practice has taken the difficult decision that any requests from specialists, both NHS and private, to prescribe ADHD medications to adult patients, will be declined. Also, we will no longer be able to supply ADHD medicines safely to adult patients who have obtained these medicines from the practice in the past. We will be making this clear to providers of ADHD services, at the point we refer patients for a diagnostic assessment.
Care of adults already receiving ADHD treatments remains under careful review. Patients may be able to access the care they need outside of the NHS, for instance by seeking a referral to a private provider from their NHS GP or NHS specialist. As your NHS GP, we will not enter into “shared care” arrangements with private providers.
The practice feels strongly that patients should not be left without the care they need, due to a lack of comprehensive NHS funding, and our local representatives have raised this issue with local funding and decision-making groups. By taking this stand with other Oxfordshire GP practices we hope that a safe service will be funded.
If you also wish to raise this issue, please contact the “planned care team” at BOB ICB, This email address is being protected from spambots. You need JavaScript enabled to view it., and/or your MP.
We understand that some of our patients may have been unable to view certain documents (e.g. letters from the hospital) when using online services due to a software problem.
We sincerely apologise for any inconvenience this may have caused.
We are pleased to inform you that this issue has been resolved; any new documents added to your electronic GP health records will be visible and it may take up to a month for older, affected documents to become visible.
Your GP team will have been able to access the letters, so your care will not have been affected during this time.
If you have been contacted by the NHS saying you/your child may not be up to date with their MMR vaccinations but you think they are, please be assured, we are aware that data held nationally may differ from what is held locally and NHS England continues to work with NHS services delivering vaccinations to ensure that patient records are as up to date as possible.
If you are satisfied that you/your child is up to date for MMR vaccination and other childhood vaccination and the general practice are satisfied that the practice record is complete, then no further action is necessary.
Pharmacy First
Pharmacists can give you advice on a range of conditions and suggest medicines that can help.
They may also be able to offer treatment and some prescription medicine for some conditions, without you needing to see a GP (this is called Pharmacy First). Conditions they can treat as part of Pharmacy First are :-
- Sinusitis - For adults and children aged 12 and over
- Sore throat - For adults and children aged 5 and over
- Earache - For children aged 1 - 17 years
- Infected insect bite - For adults and children aged 1 year and over
- Impetigo (a bacterial skin infection) - For adults and children aged 1 year and over
- Shingles - For adults aged 18 and over
- Uncomplicated urinary tract infections in women - Women aged 16 to 64 years
How can I access treatment from my pharmacy?
You can get treatment for these conditions by walking into the pharmacy. You do not need to be referred from your GP Surgery.
If you go to a pharmacy with one of these conditions, the pharmacist will offer you advice, treatment or refer you to a GP or other healthcare professional if needed.
They will then update your GP health record.
If you are not within these age ranges, a pharmacist can still offer advice, but you may need to see a GP for treatment.
Pharmacy First Services - My Local Surgery
The pharmacies in Witney which are offering the Pharmacy First Service are :-
Witney Pharmacy
Boots High Street
Boots Edington Square
Please click HERE to read the Patient Charter
HERE are some to tips for Veterans

If your child hasn’t had one or both doses of measles, mumps and rubella (MMR) which helps protect them against these potentially serious illnesses please contact Reception to book their appointment
To find more information about the MMR vaccine here: www.nhs.uk/mmr and https://vaccineknowledge.ox.ac.uk/mmr-vaccine
As a practice we are always looking to improve our ability to communicate with our patients so would like to encourage all smart phone users to download the NHS APP this will allow you easy access to your medical records for results and ordering repeat medication.
For more information on how to download the app please following the website: https://www.nhs.uk/using-the-nhs/nhs-services/the-nhs-app/
We would also like to ensure we have up-to-date contact details on your health records, so please call Reception if any details have changed or you need to add an email address/mobile number.
Due to increased workloads within the Practice, we are not able to guarantee that Prescription requests will be processed within 5 working days. We are now advising patients to allow 5 working days for prescriptions to be processed and sent to their nominated pharmacy.
In line with current recommendations from the BMA (British Medical Association) and LMC (local medical committee), we have opted out of the proposed enhanced patient access for the time being, due to safety concerns for some of our patients. Please see attached link from the BMA which explains why we have taken this decsion. We will update you when we get any more information.
Accelerated access to GP-held patient records guidance (bma.org.uk)
FEAR OF FLYING
Patients come to us, asking us to prescribe diazepam for fear of flying. There are a number of very good reasons why prescribing this drug is not recommended.
1) Diazepam is a sedative, which means it makes you sleepy and more relaxed. If there is an emergency during the flight it may impair your ability to concentrate, follow instructions and react to the situation. This could have serious safety consequences for you and those around you.
2) Sedative drugs can make you fall asleep, however when you do sleep it is an unnatural non-REM sleep. This means you won’t move around as much as during natural sleep. This can cause you to be at increased risk of developing a blood clot (DVT) in the leg or even the lung. Blood clots are very dangerous and can even prove fatal. This risk is even greater if your flight is greater than 4 hours.
3) Whilst most people find benzodiazepines like diazepam sedating, a small number have paradoxical agitation and increased aggression. They can also cause disinhibition and lead you to behave in a way that you would not normally. This could impact on your safety as well as that of other passengers and could also get you into trouble with the law.
4) According to the prescribing guidelines doctors follow (BNF) Benzodiazepines are contraindicated (not allowed) in treating phobia. Your doctor would be taking a significant legal risk by prescribing against these guidelines. They are only licensed short term for a crisis in generalised anxiety. If this is the case, you should be getting proper care and support for your mental health and not going on a flight.
5) Diazepam and similar drugs are illegal in a number of countries. They may be confiscated or you may find yourself in trouble with the police.
6) Diazepam stays in your system for quite a while. If your job requires you to submit to random drug testing you may fail this having taken diazepam.
We appreciate that fear of flying is very real and very frightening. A much better approach is to tackle this properly with a Fear of Flying course run by the airlines. We have listed a number of these below.
What is changing:
There will be an ability now to pre-book appointments with GP in the future: both phone and face to face.
You no longer need to phone up on a specific day that your GP is in.
Online “e-consults” will be available Monday - Thursday from 18:30 to 21:00, and on a Sunday from 16:30 - 21:00.
We are being more transparent with our patients about our capacity for GP appointments, and aligning our work patterns with the BMA’s statement on safe working in General Practice. (https://www.bma.org.uk/advice-and-support/gp-practices/managing-workload/safe-working-in-general-practice)
Individual GPs are also spreading their capacity throughout the week.
Why is this changing:
Prior to the COVID-19 pandemic we changed our appointment system by having all requests for GP appointments to be triaged first (usually by telephone). This was in response to patient complaints that the wait for appointment was too long. By triaging appointments and dealing with as much as we could remotely, we increased our throughput of consultations with patients receiving GP care far quicker than before. As it happens, the nature of the COVID-19 pandemic prompted GP practices nationally to adopt a similar system for differing reasons.
However, the need to phone was frustrating for patients and the volume of work was exhausting for our GP staff.
Most of our GPs work 10-12 hours a day a week, mostly 3 days a week or more, with additional hours working from home when not at the surgery doing important work which is not directly patient facing but vital for patient care. This works out at around what most people would regard as “full time” over the course of a week. On a typical day in our old system any one GP may have 30 to 60 patient contacts (mainly by phone). This is more than the BMA’s recommendations on safe working intensity for GPs. We have three to five GPs in on any one day.
What is not changing:
There will still be an element of telephone or online triage, especially for on the day capacity and to manage demand for appointments generally. The central problem has not changed: the demand for GP time is beyond the capacity we have to provide GP appointments. It is therefore envisaged that the wait for appointments booked in advance will run to several weeks.
We continue to encourage patients to self care were possible and seek alternatives to GP appointments where more appropriate.
Our GP mostly continue to work the equivalent of full time (approximately 37.5 hrs a week) over 3 or more days a week.
What we are continuing to do:
We are continuing to monitor how our appointment system works, and are seeking to expand our clinical workforce. Frustratingly, there is a recruitment and retention problem nationally with GPs. We are also seeking to expand our workforce to support our existing GP according to government's additional roles initiative as part of working in a Primary Care Network (PCN).
This practice is supporting vital health and care planning and research by sharing your data with NHS Digital. For more information about this see the GP Practice Privacy Notice at:
NHS Digital's own website.
Note that consent to have your data shared in this way is automatic unless you opt out.
What Data is Shared
Data may be shared from the GP medical records about:
- any living patient registered at a GP practice in England when the collection started - this includes children and adults
- any patient who died after 1 July 2021, and was previously registered at a GP practice in England when the data collection start
NHS Digital will not collect patients’ names or addresses. Any other data that could directly identify patients (such as NHS Number, date of birth, full postcode) is replaced with unique codes which are produced by de-identification software before the data is shared with NHS Digital.
This process is called pseudonymisation and means that patients will not be identified directly in the data. NHS Digital will be able to use the software to convert the unique codes back to data that could directly identify patients in certain circumstances, and where there is a valid legal reason.
To Opt out Of Data Sharing
If you would prefer that your identifiable patient data is only shared for your own health care purposes, you can opt-out by registering a Type 1 Opt-out or a National Data Opt-out, or both.
These opt-outs are different and they are explained in more detail in below. Your individual care will not be affected if you opt-out using either option (or both).
A Type 1 opt out has to be registered by your Practice; please let us know if you want to register a type 1 opt out.
A National Opt out can be done without contacting your practice, at https://www.nhs.uk/your-nhs-data-matters/
Type 1 Opt-out (opting out of NHS Digital collecting your data)
NHSD will not collect data from GP practices about patients who have registered a Type 1 Opt-out with their practice. More information about Type 1 Opt-outs is in the GP Data for Planning and Research Transparency Notice, including a form that you can complete and send to your GP practice.
The collection started on 1 July 2021 so if you do not want your data to be shared with NHS Digital, please register your Type 1 Opt-out with your GP practice.
If you register a Type 1 Opt-out after this collection has started, no more of your data will be shared with NHSD. They will however still hold the patient data which was shared before you registered the Type 1 Opt-out.
If you do not want NHS Digital to share your identifiable patient data with anyone else for purposes beyond your own care, then you can also register a National Data Opt-out.
You can download a blank form here which you can then send to us by post or email.
National Data Opt-out (opting out of NHS Digital sharing your data with other organizations)
NHSD will collect data from GP medical records about patients who have registered a National Data Opt-out. The National Data Opt-out applies to identifiable patient data about your health, which is called confidential patient information.
NHS Digital won’t share any confidential patient information about you - this includes GP data, or other information, such as hospital data - with other organisations, unless there is an exemption to this.
To find out more information and how to register a National Data Opt-Out, please read NHSD GP Data for Planning and Research Transparency Notice.

If you’re a patient at our practice you can now use the new NHS App, a simple and secure way to access a range of NHS services on your smartphone or tablet.
You can use the NHS App to check your symptoms and get instant advice, book appointments, order repeat prescriptions, view your GP medical record and more.
You will also have evidence of your covid vaccinations on the App; useful for when you have to travel abroad.
If you already use any of the Patient Access providers, you can continue to use them. You can use the NHS App as well.
For more information go to www.nhs.uk/nhsapp
We have been part of the scheme for 3 years.
A map showing premises signed up to the scheme throughout West Oxfordshire can be found on the WODC website.
https://www.safeplaces.org.uk/search/?query=West%20Oxfordshire%20District%2C%20UK&exact
For more information on the scheme, please see:
https://www.westoxon.gov.uk/communities-and-leisure/community-safety/safe-places/
https://www.facebook.com/SafePlacesOxfordshire/?ref=hl
There is also an App which you can download here:
https://www.safeplaces.org.uk
Community Connect
Medicine that doesn't come in a tube or bottle!
Community Connect, a new Social Prescribing service which helps with people’s health and well-being, is now available at the Nuffield surgery. It links people with community activities to improve mental and physical wellbeing and reduce loneliness.
Social Prescribing is a way in which people living with long term conditions can get access to a variety of support services they need. Issues like help with getting a job, housing, debt management and social contact. Help with these things is often available through local authorities, charities and local community organisations.
Social Prescribing means that the individual can build their support links by working with a Community Navigator who does know, or who has expertise in finding out, what is available. Following a referral from the GP, together with the Community Navigator, the individual can discuss their problems and identify the support that they need to manage their own health more effectively and meet their own personal goals.
Get in touch: This email address is being protected from spambots. You need JavaScript enabled to view it.
Find out more at: https://www.canosn.org.uk/Pages/Category/community-connect